Understanding and Managing Pelvic Health During the Menopause Transition
Ladies,
You pelvic health is a crucial aspect of your well-being that often gets overlooked, especially during the menopause transition and beyond. Understanding the changes that occur and how to manage them can significantly improve your quality of life. Today, we'll delve into the genitourinary syndrome of menopause (GSM), the importance of pelvic floor health, and effective treatments to ensure comfort and vitality during this phase.
Understanding Genitourinary Syndrome of Menopause (GSM)
Genitourinary syndrome of menopause (GSM) is a term that describes the range of symptoms caused by decreased estrogen and other sex steroids during menopause. GSM affects about 50-70% of postmenopausal women and can also occur in other low estrogen states, such as postpartum and breastfeeding. Symptoms include vaginal dryness, burning, irritation, urinary urgency, frequency, and recurrent urinary tract infections (UTIs).
Understanding Hormones
Hormones are like the body’s internal magic wand, transforming tissues and functions as we grow and age. During childhood, the absence of hormones leaves vulvar tissues thin and sensitive. Puberty introduces estrogen, leading to significant changes in genital tissue, making it pink, stretchy, and lubricated. However, as menopause approaches, the decline in estrogen causes these tissues to revert to a more vulnerable state.
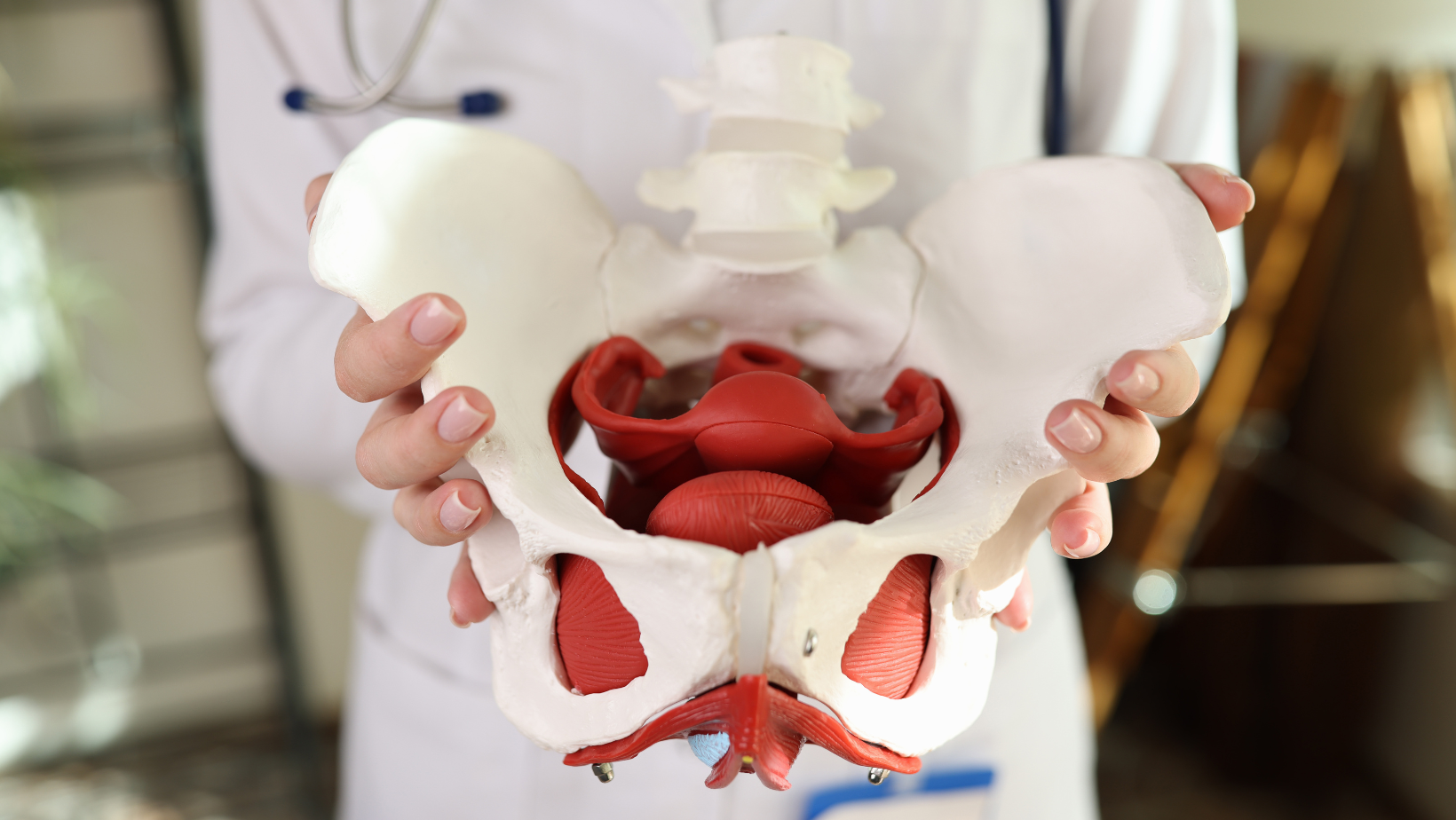
Pelvic Anatomy and Hormone Receptors
The pelvic floor is a network of muscles, ligaments, and tissues supporting the bladder, uterus, and rectum. Estrogen and testosterone receptors are abundant in these tissues. Declining hormone levels lead to several changes:
- pH Changes: The vaginal pH becomes more alkaline, disrupting the natural flora and increasing infection risk.
- Tissue Atrophy: Vaginal tissues become thinner, less elastic, and more prone to tears and irritation.
- Anatomical Shifts: The urethra can move closer to the vaginal opening, contributing to urinary symptoms and recurrent UTIs.
The Severe Implications of Recurrent UTIs
Recurrent UTIs are a common and severe implication of GSM. These infections can lead to chronic discomfort, frequent antibiotic use, and significant impact on quality of life. Ensuring the health of vaginal and urinary tissues is crucial in preventing these infections & can be life saving.
Effective Treatments for GSM
Suffering from GSM is not normal, and there are safe and effective treatments available. Vaginal estrogen therapy is highly effective and has minimal contraindications. Unlike systemic hormone replacement therapy (HRT or MHT (menopausal hormone therapy), vaginal estrogen is not absorbed significantly into the bloodstream and specifically targets affected tissues.
Benefits of Vaginal Estrogen:
- Restores natural pH and flora
- Increases tissue elasticity and moisture
- Reduces urinary symptoms and the risk of UTIs
Systemic estrogen therapy with HRT/MHT is not always effective at treating GSM, and many women require topical estrogen treatment for relief.
Lubricants and Moisturizers
Using vaginal lubricants and moisturizers can also help manage GSM symptoms. Lubricants are used during sexual activity to reduce friction, while moisturizers are used regularly to maintain vaginal moisture. When using silicone-based toys, avoid silicone lubricants as they can degrade the material.
Pelvic Floor Dysfunction
Pelvic floor dysfunction involves abnormal activity or function of pelvic floor muscles, leading to urinary incontinence, pelvic pain, and discomfort during intercourse. It’s essential to understand that pelvic floor dysfunction can result from both weakened and overly tight pelvic muscles.
Pelvic Floor Physical Therapy:
- Addresses both weakness and excessive tightness
- Helps restore normal function and alleviate symptoms
- Provides education on proper techniques, as many women do not perform Kegel exercises correctly
Normalizing Pelvic Health Discussions
It’s essential to normalize conversations about pelvic health. This aspect of our health is not taboo but a crucial part of our overall well-being. Even women who no longer need Pap smears should have regular vaginal exams to monitor and maintain pelvic health.
Encourage yourself to be comfortable with your anatomy and seek care from clinicians who are knowledgeable and comfortable discussing and treating pelvic health issues.
Conclusion
Maintaining pelvic health during the menopause transition and beyond is vital for overall well-being. Understanding GSM, utilizing effective treatments like vaginal estrogen, and seeking pelvic floor physical therapy can significantly improve your quality of life. Embrace this phase with knowledge and confidence, ensuring that your health and comfort are prioritized.
Additional Insights and Tips
- Estrogen Therapy Safety: There is no data indicating that local vaginal estrogen causes cancer, cardiovascular problems, stroke, or dementia. Studies with over 18 years of observational data show its safety. Even for women with a history of gynecologic cancers, local vaginal estrogens are considered safe.
- Long-term Use: Just like brushing your teeth or moisturizing your skin, using vaginal estrogen is a long-term commitment. It works as long as you keep using it, so it's important to continue the therapy even after symptoms improve.
- Options for Application: Vaginal estrogen comes in various forms, including creams, inserts, and rings. It may take up to 2-3 months to see the full benefits, but consistency is key.
- Pelvic Floor Therapy: Not all pelvic floor dysfunctions are due to weakness. Some are due to excessive tightness. A specialized pelvic floor physical therapist can help determine the right exercises and treatments.
- Seek Expert Care: Ensure your healthcare provider is comfortable and knowledgeable about pelvic health. Regular exams and open discussions about any symptoms are crucial.
Embrace this phase with knowledge and confidence, ensuring that your health and comfort are prioritized.
We got this!
Dr. Anna
WonderCreek Health Blog



